Cryoablation
Cryoablation For Prostate Cancer
Cryotherapy (or cryosurgery / cryoablation) is a minimally-invasive effective treatment for prostate cancer with fewer side-effects than a radical prostatectomy or radiation therapy.
What is Cryotherapy ?
Cryoablation consists of rapid freezing and slow thawing to induce tissue shearing, as well as rupturing of cell membranes, organelles and the cytoskeleton, leading to secondary anoxia and tissue necrosis, and is used in many branches of surgery. In the first cryosurgery device, invented by Irving S. Cooper, who was an assistant professor of neurosurgery at the New York University School of Medicine in 1952, liquid nitrogen was used to focally freeze the thalamus to treat tremors in patients with Parkinson disease. In 1964, cryotherapy with liquid nitrogen was used to treat prostate cancer. However, the adoption of this technology failed at that time, owing to poor control of the edge of the ice ball, which led to unacceptably high rates of rectal fistula and incontinence.
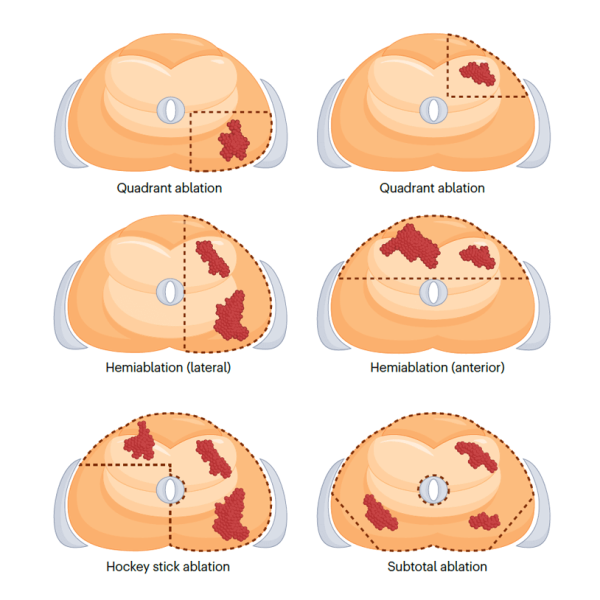
The introduction of small cryotherapy probes, grid-based templates and use of argon rather than liquid nitrogen facilitated rapid freezing with improved precision, resulting in the re-emergence of cryoablation in the late 1990s. The likelihood of urethral sloughing also decreased with the use of a urethral warming catheter. Moreover, the use of a transrectal ultrasound probe enabled surgeons to track the edge of the ice ball, which helped prevent inadvertent damaging of important structures, such as the rectum and the urethral sphincter. Subsequently, disease localization with prostate MRI enabled targeted biopsy and provided the impetus for partial gland ablation (PGA) using focal therapy, particularly cryoablation.

